Real Stories: How Women Beat Weight Gain with Lean and Insulin-Resistant PCOS

Have you ever wondered why losing weight feels almost impossible when you have PCOS, even when you are doing everything right?
TL;DR - PCOS Weight Management Guide
Who it's for: Women with lean PCOS or insulin-resistant PCOS struggling with weight management and symptoms
Main outcomes: Understanding your PCOS type, personalized diet strategies, real success stories with measurable results
Key approach: Pair carbs with protein at every meal, track your food patterns, focus on blood sugar stability
Timeline: Energy improvements in 2-4 weeks, menstrual regularity in 2-3 months, significant results in 3-6 months
Safety note: Consult your doctor before making major dietary changes, especially if you have other health conditions
IMPORTANT
Your PCOS nutrition plan at a glance.
A quick roadmap so you can act fast.
⏱️ Progress 0/4 - ~0 minutes in - Keep going
⏳ Understand: Learn the 2 PCOS types and why they matter
⏳ Case Studies: 3 real women, 3 different PCOS journeys
⏳ Action Plan: 7 tips + 7-step meal plan guide
🔍 The one habit all 3 women discovered independently (revealed in Tip 5)
I remember meeting Priya, a 28-year-old software developer from Bangalore, who cried in frustration because the scale would not budge despite eating salads and going to the gym five times a week. She had lean PCOS - her BMI was 23 - but she still struggled with stubborn belly fat and irregular periods. Her doctor had told her she was "fine" because she was not overweight.
Then there was Meera, a 34-year-old teacher from Mumbai, who had classic insulin-resistant PCOS. She had tried keto, intermittent fasting, and every diet plan on the internet. Nothing worked for more than a few weeks. She felt like her body was fighting against her.
Both women had PCOS. Both struggled with weight. But their paths to feeling better were completely different.
This is what makes PCOS so tricky - it is not one condition but a spectrum of conditions. And what works for one woman might make things worse for another.
In this blog post, I will share real case studies of women who figured out their PCOS type and found eating patterns that actually worked for them. I will also share the science behind why lean PCOS and insulin-resistant PCOS need different approaches.
Preparing balanced, PCOS-friendly meals is the foundation of managing symptoms
Understanding the Two Faces of PCOS
PCOS affects about 1 in 10 women of reproductive age worldwide. But here is something most people do not know - there are different types of PCOS, and each type needs a different approach.
Understanding the differences between lean PCOS and insulin-resistant PCOS is crucial for effective management
What is Lean PCOS?
Lean PCOS affects women who have a normal BMI (under 25) but still show PCOS symptoms. About 20% of women with PCOS fall into this category. A 2024 study presented at the Pediatric Endocrine Society Annual Meeting found that adolescents with lean PCOS actually showed greater insulin resistance and adipose tissue dysfunction compared to those without PCOS, even with normal weight.
The Hidden Challenge
Many doctors miss lean PCOS diagnosis because they associate PCOS with being overweight. Women with lean PCOS often hear phrases like "you look healthy" or "just lose a few pounds" when weight loss is not even the issue.
Research published in the journal Human Reproduction shows that insulin resistance is inherent in PCOS independent of obesity. This means even thin women can have blood sugar issues that affect their hormones.
What is Insulin-Resistant PCOS?
Insulin-resistant PCOS is the most common type, affecting roughly 70% of women with the condition. In this type, the body does not use insulin properly. When cells become less responsive to insulin, the pancreas makes more of it. High insulin then tells the ovaries to make extra testosterone, which causes many PCOS symptoms like acne, facial hair, and weight gain around the middle.
According to Johns Hopkins Medicine, insulin resistance affects 50% to 75% of all people with PCOS. A clinical dietitian at Johns Hopkins explains that when insulin does not convey glucose into cells properly, the body keeps making more insulin, creating a cycle that is hard to break.
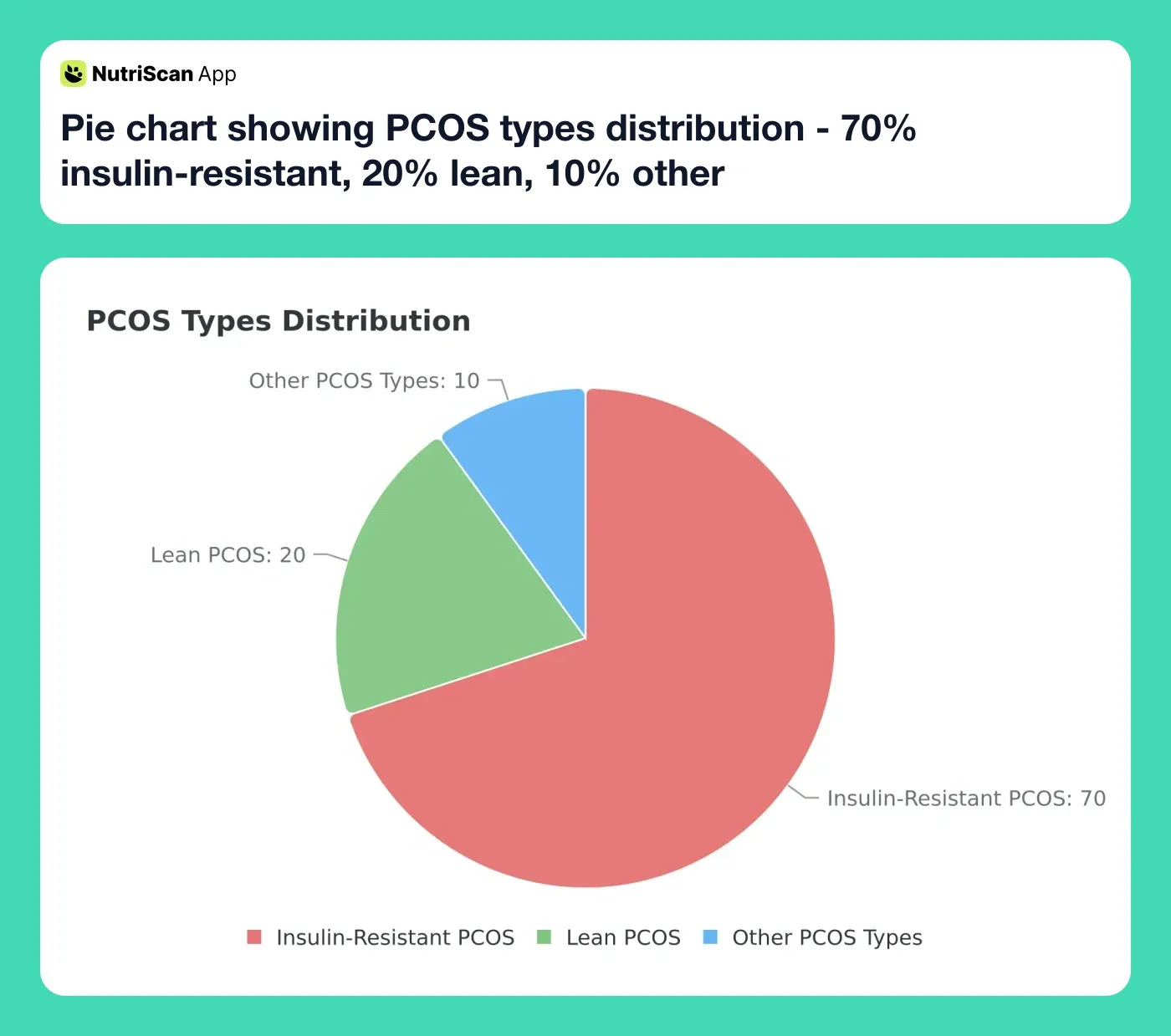
Figure 1: Distribution of PCOS types among women with the condition
IMPORTANT
Checkpoint: here's where you are right now.
Quick status update so you always know the next best move.
⏱️ Progress 1/4 - ~1 minute in - Keep going
✅ Understand: PCOS types explained (done)
👉 Case Studies: 3 real journeys (you're here)
⏳ Action Plan: 7 tips + meal plan guide
🧩 The one habit all 3 women share (coming soon)
Case Study 1: Priya's Path with Lean PCOS
Background:
- Age: 28
- BMI: 23
- PCOS Type: Lean PCOS
- Main Symptoms: Irregular periods, acne, belly fat despite normal weight, fatigue
The Problem:
Priya had been diagnosed with PCOS at age 24. But because she was not overweight, her doctor simply put her on birth control pills and said to "watch her diet." For four years, she struggled with energy crashes after meals, stubborn acne, and periods that came whenever they wanted.
She was eating what she thought was healthy - fruit smoothies for breakfast, sandwiches for lunch, and dal-rice for dinner. She avoided fried foods and rarely ate sweets. So why was her body still fighting her?
What She Discovered:
After tracking her meals and how she felt after eating, Priya noticed a pattern. Every time she had a carb-heavy meal without enough protein, she felt exhausted an hour later. Her morning fruit smoothie, which she thought was healthy, was actually spiking her blood sugar because it had no protein or fat to slow down digestion.
Key Insight
Research from the Journal of Clinical Endocrinology and Metabolism shows that many lean women with PCOS have completely normal fasting insulin levels, but they secrete much more insulin after eating glucose. This means standard diabetes tests might look normal, but their bodies still overreact to carbs.
The Changes She Made:
Started pairing carbs with protein: Instead of fruit smoothies, she switched to eggs with vegetables and a small portion of fruit on the side.
Focused on quality over quantity: She did not cut calories - she just reorganized her plate to include protein, healthy fats, and fiber at every meal.
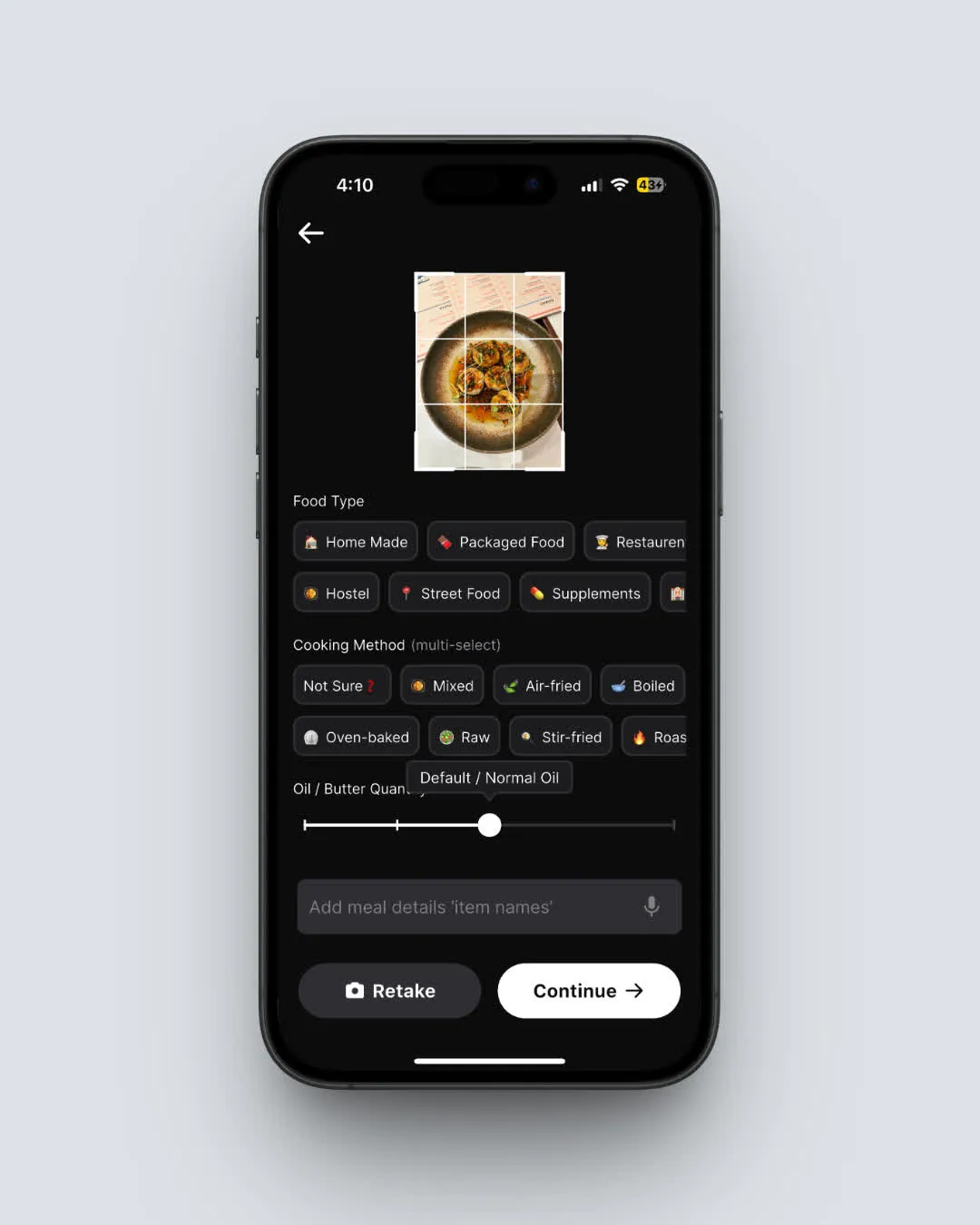
Started tracking her food: Using a meal tracking app, she photographed every meal and noticed patterns in how different foods affected her energy and symptoms.
Added strength training: Research shows that building lean muscle mass improves insulin sensitivity even in women with normal weight.
The Results After 6 Months:
Priya's periods became regular for the first time in years. Her acne cleared up significantly. She lost 3 kg of belly fat even though her overall weight stayed almost the same - her body composition changed. Most importantly, she had steady energy throughout the day instead of the crashes she used to experience.
Case Study 2: Meera's Battle with Insulin-Resistant PCOS
Background:
- Age: 34
- BMI: 31
- PCOS Type: Insulin-Resistant PCOS
- Main Symptoms: Weight gain (especially around belly), facial hair, irregular periods, dark skin patches on neck
The Problem:
Meera had gained 25 kg over 10 years despite being very active in her twenties. She had tried every diet - keto, paleo, intermittent fasting - and while she would lose weight initially, it always came back. Plus more.
Her doctor had warned her about pre-diabetes. Her fasting blood sugar was borderline high, and her insulin levels were elevated. She felt like she was fighting a losing battle with her own body.
What She Discovered:
When Meera started really looking at what she was eating - not just the macros but the actual foods - she realized several things:
She was eating "healthy" foods that were actually high in hidden sugars (flavored yogurts, protein bars, store-bought smoothies)
She often skipped meals during the day, then ate a large dinner because she was starving
Her stress levels were through the roof, which was raising her cortisol and making insulin resistance worse
A meta-analysis published in the Journal of Clinical Nutrition analyzed 19 trials with 1193 participants and found that diet significantly improved insulin resistance and body composition in PCOS patients. The DASH diet and calorie-restricted diets showed the most promise.
The Changes She Made:
Stopped skipping meals: She started eating smaller, balanced meals every 4-5 hours to keep blood sugar stable. Mass General Brigham researchers recommend planning meals at times when they can actually fuel activity.
Cut out hidden sugars: She started reading labels carefully and realized her "healthy" breakfast cereal had more sugar than a chocolate bar.
Added more fiber and protein: She increased vegetables to cover half her plate and made sure each meal had a good protein source.
Started walking after meals: A 15-minute walk after dinner helped her body use the glucose from her meal more effectively.
Prioritized sleep: She went from 5-6 hours to 7-8 hours of sleep, which research shows helps regulate hunger hormones.
Tracked everything: She used a nutrition tracking app to photograph meals and see exactly what she was eating. This helped her catch the sneaky sources of sugar she had been missing.
The Results After 8 Months:
Meera lost 12 kg - and kept it off for over a year now. Her fasting blood sugar returned to normal range. Her periods became regular. The dark patches on her neck started fading. She says the biggest change was not physical - it was mental. She finally felt in control of her body instead of fighting it.

Figure 2: Weight loss results from our three case studies over their journey periods
IMPORTANT
Checkpoint: midway progress update.
You're halfway - the patterns start to emerge here.
⏱️ Progress 2/4 - ~2 minutes in - Keep going
✅ Understand: PCOS types (done)
✅ Case Study 1: Priya - Lean PCOS (done)
✅ Case Study 2: Meera - Insulin-Resistant PCOS (done)
👉 Case Study 3: Sunita - Mixed type (current)
🧩 The one habit all 3 share - can you spot it yet? (coming soon)
Case Study 3: Sunita's Story - From Diagnosis to Diet Plan
Background:
- Age: 31
- BMI: 27
- PCOS Type: Mixed (some insulin resistance with lean PCOS features)
- Main Symptoms: Difficulty getting pregnant, mild acne, irregular cycles
The Problem:
Sunita and her husband had been trying to conceive for two years. After multiple tests, she was diagnosed with PCOS. Her doctor suggested medication, but Sunita wanted to try lifestyle changes first.
Her case was interesting because she fell somewhere between lean and insulin-resistant PCOS. Her BMI was slightly elevated, but her main issue was irregular ovulation rather than severe metabolic problems.
What She Discovered:
Research from Smart Fertility Choices shows that the right PCOS diet addresses the underlying drivers of all PCOS symptoms - inflammation and poor blood sugar regulation. By targeting these root causes, women can improve not just weight but also fertility, skin health, and mood.
Sunita learned that even losing 5% of body weight can significantly improve insulin resistance, hormone levels, menstrual cycles, and fertility in people with PCOS.
The Changes She Made:
Adopted a Mediterranean-style eating pattern: Rich in vegetables, fish, olive oil, nuts, and whole grains - this approach has been shown to improve insulin sensitivity in PCOS patients.
Reduced dairy intake: One study indicated that drinking milk has a direct effect on people with PCOS, and reducing dairy might help reduce symptoms.
Cut gluten and processed foods: Many women with PCOS report that going gluten-free helps with inflammation and bloating.
Added specific supplements: After consulting her doctor, she started inositol and omega-3s, which show promise in PCOS research.
Used food tracking to understand her patterns: By photographing and logging meals, she could see what combinations made her feel best.
The Results After 10 Months:
Sunita lost 6 kg. Her cycles became regular - every 28-32 days instead of the random 45-90 day cycles she had before. And the big news? She got pregnant naturally after 10 months of dietary changes, without needing fertility medication.

The moment when all your hard work pays off - celebrating health victories

7 Actionable Tips for Managing PCOS Through Nutrition
Based on the case studies and research, here are the most effective strategies:
Tip 1: Know Your PCOS Type
Before changing anything, understand what type of PCOS you have. Get a complete hormone panel and insulin test - not just fasting glucose, but also fasting insulin. If your doctor only checks fasting glucose, ask specifically for insulin levels too.
Tip 2: Pair Every Carb with Protein
This is the golden rule for PCOS nutrition. Never eat carbs alone. Having protein and fat with carbohydrates slows down digestion and prevents blood sugar spikes that trigger insulin surges.
Examples:
- Apple alone becomes Apple with almond butter
- Rice alone becomes Rice with dal and vegetables
- Fruit smoothie alone becomes Smoothie with protein powder and nut butter
Tip 3: Prioritize Fiber at Every Meal
Fiber slows glucose absorption, helping prevent blood sugar spikes. Aim for at least 25-30 grams of fiber daily from vegetables, legumes, and whole grains. Mass General Brigham recommends filling half your plate with non-starchy vegetables at every meal.

Figure 3: The ideal PCOS-friendly plate composition for balanced blood sugar
Tip 4: Time Your Meals Right
Eating when you are most active helps your body use glucose more effectively. This means eating a proper breakfast and lunch rather than skipping meals and eating a huge dinner. Research shows this approach helps maintain stable blood sugar and insulin levels.
IMPORTANT
Checkpoint: final stretch before the reveal.
One last nudge - the habit all 3 women share is next.
⏱️ Progress 3/4 - ~3 minutes in - Keep going
✅ Understand: PCOS types
✅ 3 Case Studies: Priya, Meera, Sunita
✅ Tips 1-4: PCOS type, protein pairing, fiber, meal timing
✨ The universal habit - about to reveal
Tip 5: Track Your Food to Find Your Patterns
You cannot fix what you cannot see. Photographing and logging your meals helps you:
- Spot hidden sources of sugar
- Notice how different foods affect your energy
- See if you are actually eating balanced meals
- Track progress over time
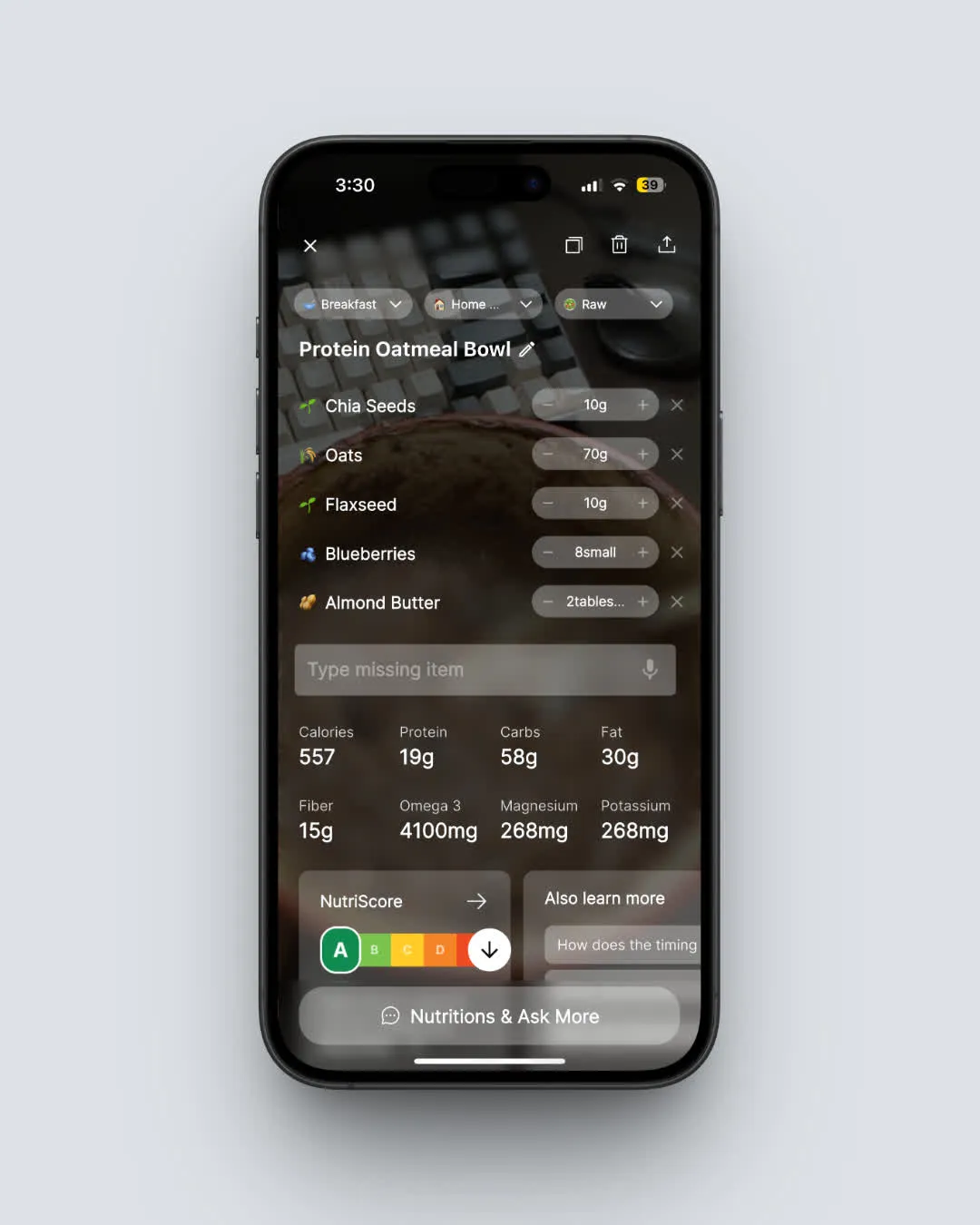
With NutriScan, you can simply snap a photo of your meal and get instant nutrition analysis. The app shows you calories, protein, carbs, fat, and even micro-nutrients. Plus, you can ask questions about your eating patterns through the NutriBites feature - like "why am I always tired after lunch?" and get insights based on your actual meal history. For women with PCOS, the PCOS Macro Calculator helps determine your personalized protein, carb, and fat targets.
Tracking your meals with a simple photo helps identify patterns affecting your PCOS symptoms
Tip 6: Do Not Fear Healthy Fats
Healthy fats from avocado, olive oil, nuts, and fatty fish help improve insulin sensitivity. Research shows that the Mediterranean-style fat profile helps reduce chronic inflammation linked to PCOS.
Tip 7: Focus on Progress, Not Perfection
Every woman in our case studies had setbacks. Priya still eats birthday cake. Meera sometimes has pizza. Sunita occasionally skips her supplements. The key is consistency over time, not perfection every day.
Step-by-Step Guide: Creating Your PCOS-Friendly Meal Plan
Step 1: Assess Your Current Eating
For one week, track everything you eat without changing anything. This gives you a baseline. Look at:
- How many meals contain protein?
- How often do you eat carbs alone?
- What are your biggest sources of added sugar?
- How do you feel after different meals?
Step 2: Identify Your Personal Triggers
Not all carbs affect everyone the same way. Some women with PCOS can handle oats perfectly but feel terrible after white rice. Others are fine with rice but struggle with bread. Your food tracking data will show you your personal trigger foods.
Step 3: Plan Your Protein Sources
Make a list of proteins you enjoy and can prepare easily. Include:
- Animal proteins: Eggs, chicken, fish, paneer
- Plant proteins: Lentils, chickpeas, tofu, tempeh
- Quick options: Greek yogurt, protein powder, cottage cheese
Step 4: Build Your Vegetable Repertoire
List vegetables you actually like eating. Having options makes it easier to fill half your plate with vegetables at each meal. Include:
- Leafy greens: Spinach, kale, lettuce
- Cruciferous: Broccoli, cauliflower, cabbage
- Colorful options: Bell peppers, tomatoes, carrots
- Favorites from your cuisine: Bhindi, lauki, turai
Step 5: Choose Your Healthy Fats
Stock up on healthy fat sources:
- Cooking: Olive oil, coconut oil
- Toppings: Nuts, seeds, avocado
- Fish: Salmon, sardines, mackerel
Step 6: Create Meal Templates
Instead of planning every meal, create templates you can mix and match:
Breakfast Template: Protein (eggs/paneer/yogurt) + Fat (nuts/seeds/oil) + Fiber (vegetables/berries)
Lunch Template: Protein (dal/chicken/fish) + Complex carb (brown rice/roti) + Vegetables (half the plate) + Fat (oil/nuts)
Dinner Template: Protein + Lots of vegetables + Small portion of carbs if needed

A perfectly balanced PCOS-friendly meal following the plate composition guidelines
Step 7: Use Technology to Stay on Track
A nutrition tracking app removes the guesswork. With NutriScan for PCOS, you can:
- Photograph meals and get instant nutritional breakdown
- See your daily macro and micro-nutrient intake
- Track patterns over time through the Insights feature
- Get a personalized diet plan based on your goals (weight loss, PCOS management, etc.)
- Ask NutriBites AI questions about your eating habits
The Diet Plan feature in NutriScan Premium creates a customized plan based on your location, lifestyle, food preferences, and health goals. It considers everything from your eating schedule to any food restrictions you have.
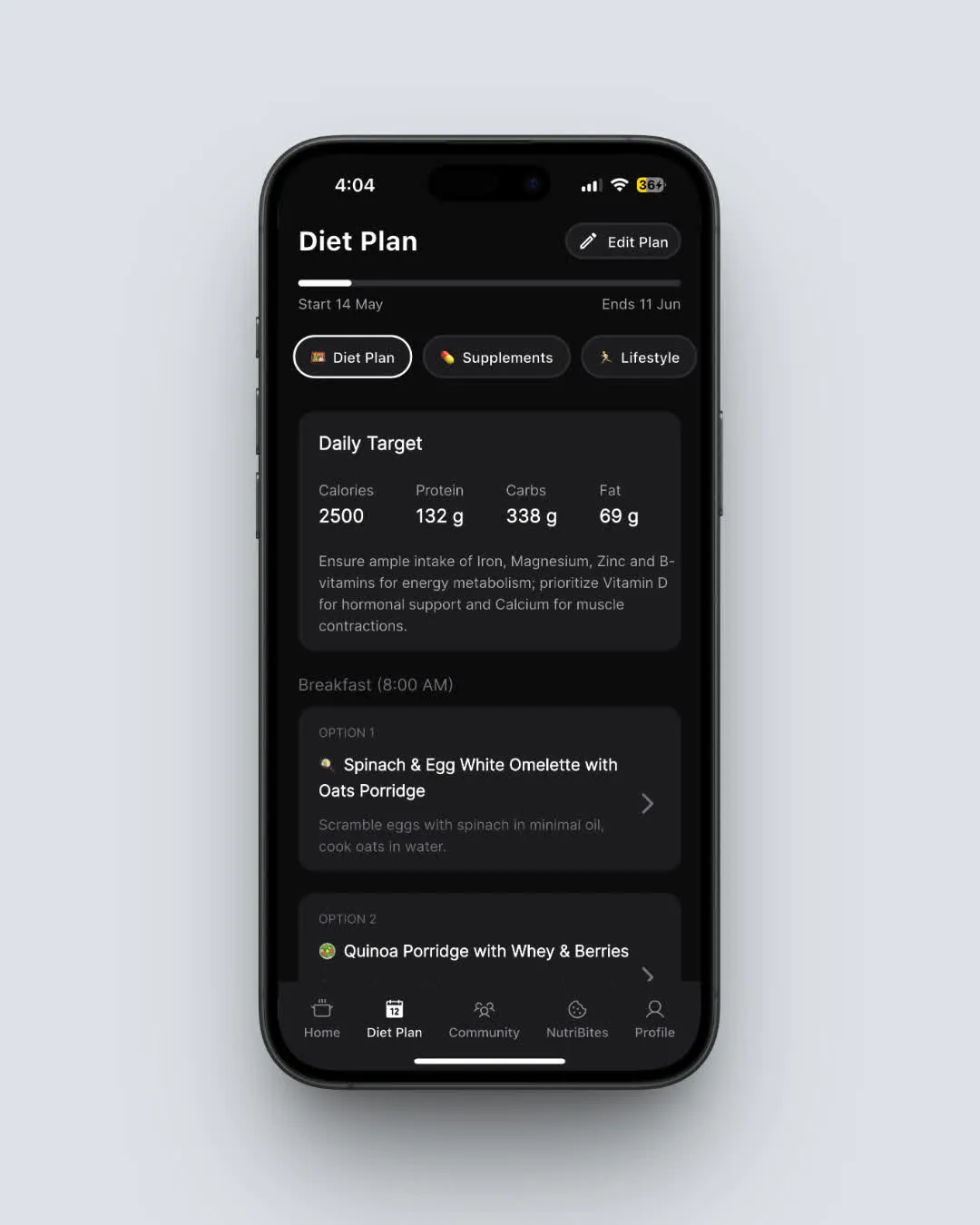
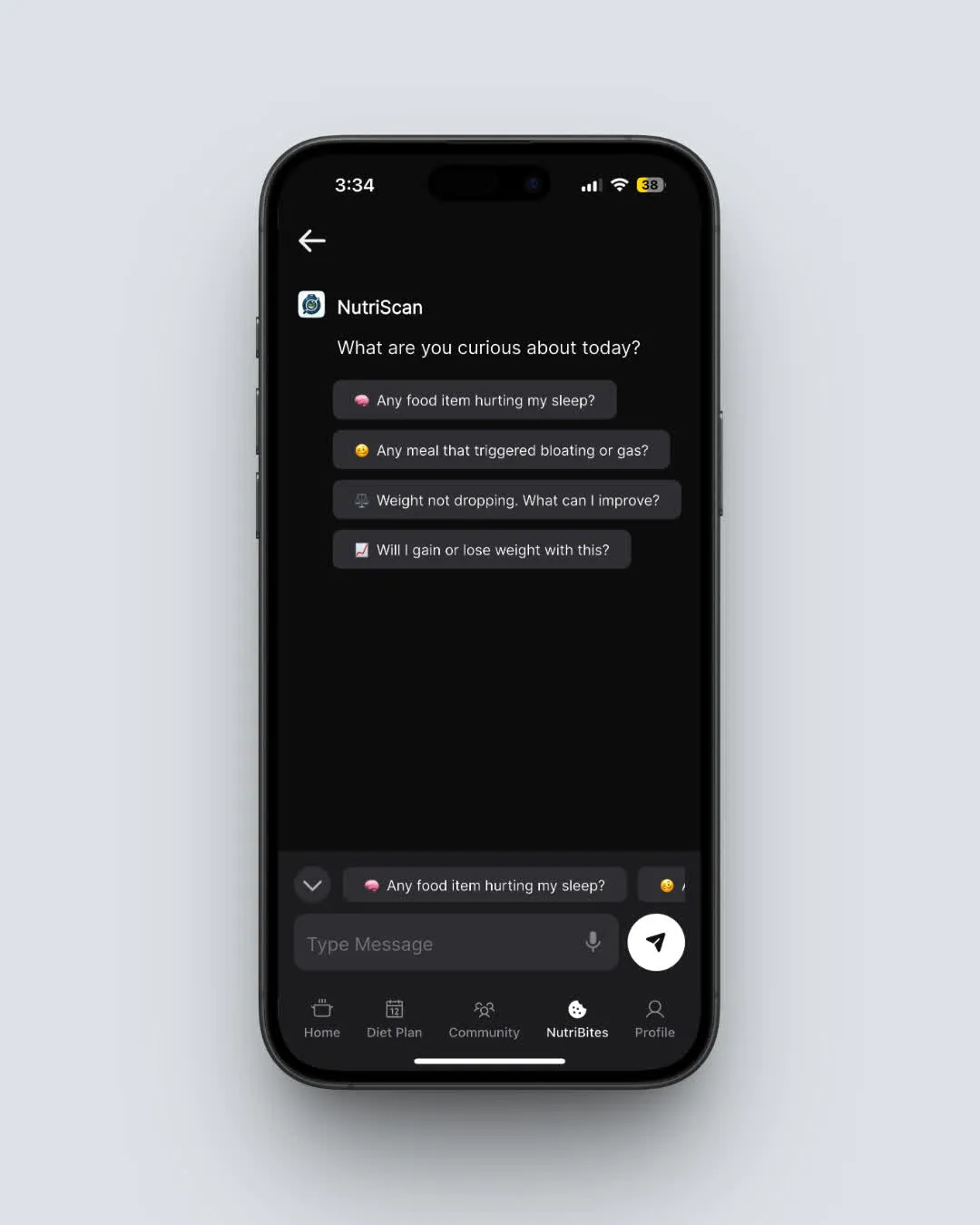

Figure 4: Expected timeline for seeing different types of improvements from diet changes
The Science Behind PCOS and Nutrition
Why Diet Matters More Than You Think
A 2020 meta-analysis in the Journal of Clinical Nutrition reviewed 19 clinical trials and found that dietary interventions significantly improved insulin resistance, fasting insulin, fasting glucose, BMI, weight, and waist circumference in PCOS patients. The researchers concluded that diet should be offered to all PCOS patients as a first-line treatment.
The Blood Sugar Connection
When you eat, your body breaks food into glucose. This glucose enters your bloodstream and signals your pancreas to release insulin. In people with insulin resistance, cells do not respond well to insulin, so the pancreas makes more and more. High insulin tells your ovaries to make testosterone, which causes many PCOS symptoms.
By eating in a way that keeps blood sugar stable, you can break this cycle.
Inflammation's Role
PCOS is associated with chronic low-grade inflammation. Certain foods - especially processed foods, refined carbs, and excess sugar - increase inflammation. Anti-inflammatory foods like vegetables, fatty fish, nuts, and olive oil help reduce it.
The Gut Connection
Emerging research shows that women with PCOS have different gut bacteria than women without the condition. Eating fiber-rich foods, fermented foods, and avoiding excess processed foods can help support a healthier gut microbiome.
Advanced: Understanding Insulin and PCOS
When insulin levels remain chronically elevated, it triggers a cascade of hormonal changes. The ovaries respond to high insulin by producing more androgens (male hormones like testosterone). This excess testosterone disrupts normal ovulation, causes acne and unwanted hair growth, and makes it harder to lose weight - especially around the midsection. Breaking this cycle through diet is one of the most effective non-pharmaceutical interventions available.
Frequently Asked Questions
Q1: Can lean women with PCOS eat more carbs than those with insulin-resistant PCOS?
Not necessarily. Research shows that even lean women with PCOS often have insulin sensitivity issues - they just do not show up on standard tests. A study found that 47% of lean women with PCOS were insulin resistant. Both lean and insulin-resistant PCOS benefit from pairing carbs with protein and choosing complex carbohydrates over refined ones. The difference is that lean women typically do not need to focus on weight loss - they need to focus on blood sugar stability and reducing inflammation.
Q2: Should I try intermittent fasting for PCOS?
Be cautious. Johns Hopkins Medicine notes that prolonged fasting can disrupt menstrual cycles and worsen blood sugar control in some women with PCOS. If you want to try it, start with a simple 12-hour overnight fast (for example, stop eating at 8 PM and eat breakfast at 8 AM). Monitor your energy, mood, and cycles carefully. Many PCOS experts recommend eating regularly throughout the day rather than fasting, as keeping blood sugar stable is key to managing PCOS.
Q3: What is the best diet for PCOS - keto, Mediterranean, or low-carb?
Research suggests the Mediterranean diet and DASH diet are most effective for improving insulin sensitivity in PCOS. These diets focus on vegetables, lean proteins, healthy fats, and whole grains without being extremely restrictive. Keto can work short-term but is hard to maintain and may not provide enough fiber for gut health. A moderate approach - reducing refined carbs and sugar while eating plenty of vegetables, protein, and healthy fats - works best for most women long-term.
Q4: How long does it take to see results from diet changes?
Most women notice energy improvements within 2-4 weeks of consistent changes. Menstrual cycle improvements often take 2-3 months. Weight loss varies but many women see meaningful progress within 3-6 months. Skin improvements (acne, dark patches) can take 4-6 months. Fertility improvements often require 6-12 months of consistent dietary changes. Be patient - PCOS took years to develop, and healing takes time.
Q5: Do I need to track my food forever?
Not forever, but tracking for at least 4-8 weeks helps you understand your patterns and learn which foods work for your body. After that, many women develop intuition about what to eat. However, periodic tracking - like one week every month - can help you stay on track and catch any unhealthy patterns that might be creeping back. Apps like NutriScan make tracking easy by letting you just photograph your meals rather than manually entering every ingredient.
IMPORTANT
Recap: everything you completed this round.
You finished the run - save this for next time.
⏱️ Progress 4/4 - ~4 minutes in - Nicely done
✅ Understand: Lean PCOS vs Insulin-Resistant PCOS
✅ 3 Case Studies: Priya (lean), Meera (insulin-resistant), Sunita (mixed)
✅ 7 Tips + 7-Step Meal Plan Guide
✅ The universal habit: Food tracking - all 3 women photographed and logged meals (revealed)
Conclusion
PCOS is not a one-size-fits-all condition, and neither is its treatment. As we have seen through Priya, Meera, and Sunita's stories, understanding your specific type of PCOS - whether lean, insulin-resistant, or a mix - is the first step to finding what works for you.
The common thread in all success stories is this: awareness leads to change. When you truly understand what you are eating and how it affects your body, you gain the power to make choices that support your health.
Here are the key takeaways:
Get proper testing - Fasting insulin, not just glucose, is essential for understanding your PCOS type
Pair carbs with protein - This simple change can make a huge difference in blood sugar stability
Track your food - You cannot change what you do not measure. Use technology to make this easier
Be patient - Lasting change takes 3-6 months minimum
Focus on patterns, not perfection - One meal will not make or break your health
Whether you have lean PCOS like Priya, insulin-resistant PCOS like Meera, or somewhere in between like Sunita, there is a path forward. The women in these case studies are not special - they simply took the time to understand their bodies and made consistent changes over time.
Your PCOS story is different, but you do not have to go through it alone. With the right tools, knowledge, and support, you can take control of your health and feel better in your body.
Start today. Snap a photo of your next meal. Notice how you feel two hours later. Write it down. This simple act of awareness is the first step toward change.
Ready to start tracking your nutrition and understanding your patterns? NutriScan for PCOS helps you photograph meals, get instant nutrition analysis, and discover insights about your eating habits. Use the PCOS Macro Calculator to find your ideal macros, then download and start your path to better health with PCOS.

 ChatGPT
ChatGPT  Claude
Claude  AI Mode
AI Mode  Perplexity
Perplexity 